General Dental Procedures by Palmetto Smiles
General Dental Procedures
Dental Cleanings
Professional cleaning by a hygienist can remove mineralized plaque that may develop even with careful brushing and flossing, particularly in complex areas to reach. This is especially true of areas below the level of the gums. Here at Palmetto Smiles, we would like to see you for a cleaning once every six months unless you have been diagnosed with periodontal disease.
How it's done: You can expect your dental cleaning to last between 30 minutes and an hour. A dental hygienist will do the professional cleaning, and Dr. Houston will come in for an exam at the end. Most people find that dental cleanings are painless and do not cause any discomfort. Anesthesia is available for patients who feel more comfortable with it.

Dental Exams and X-Rays
Beautiful smiles don’t just “happen” by chance. If you are fortunate enough to have a beautiful God-given smile, much work is involved in maintaining it for a lifetime. Routine dental exams are essential to maintaining healthy teeth and gums. Additionally, they can help avoid the financial costs associated with large treatment plans later on. Dr. Houston recommends twice yearly checkups for people of all ages. At this frequency, most problems can be caught early.
How it's done:
There are many essential components to an excellent overall exam, including:
- Medical history review: Dr. Houston and staff will assess how any medical conditions or illnesses may affect your dental health.
- Examination of tooth decay: Your mouth will be checked for cracked or decayed teeth. Often this is done with a Diagnodent laser or a Spectra camera. Each of these devices uses light to find decay and other problems. X-rays are an essential part of this exam.
- Oral cancer screening: The face, neck, lips, tongue, throat, tissues, and gums will be checked for any signs of oral cancer.
- Gum disease evaluation: Your gums and bone around the teeth will be checked for any evidence of periodontal disease.
- Examination of existing restorations: Current fillings, crowns, and other restorations are made sure to be in good order.
- T.M.J. evaluation: Your jaw joints and associated muscular structures will be evaluated.
- Radiographic evaluation: Dr. Houston will recommend diagnostic x-rays to reveal any other hidden problems, especially in the areas below the gums. Bitewing x-rays are typically taken every 12 months, and a panographic x-ray, which revolves around the head, is taken every three years.


Composite Fillings
When treating a cavity, Dr. Houston will remove the decayed portion of your tooth and fill it with another substance. This procedure is called a filling. There are multiple options for the material to be used in the filling. Amalgam and composite resin restorations are the most common.
A composite resin filling is also known as a tooth-colored filling since the material used in the filling can be closely matched to the color of your teeth. Composite fillings provide good durability for small to medium cavities. They are also particularly well suited for treating front or prominent teeth because of their natural look. Relative disadvantages of composite resin restorations include a shorter life span and more likelihood to break down for larger posterior fillings.
When can a composite filling be used for?
- Decayed tooth (i.e., cavity)
- Chipped or broken teeth
- Decreasing the gap between teeth
How it’s done: After Dr. Houston numbs the area where the filling is placed, he will remove any decayed portions of the tooth. A substance is then applied to help open up the pores of your teeth for a stronger bond and hardened and cured with a special light. Once this is complete, the filling is applied in thin layers to form the complete filling slowly. After the composite has hardened, the filling will be smoothened and polished to be comfortable and fit your bite.
Amalgam Fillings
Amalgam: Alloy of mercury and one or more other metals. Those of silver, gold, and palladium occur naturally. Those with very high mercury content are liquid; others are crystalline. Amalgams of silver and tin, with minor amounts of copper and zinc, are used in dentistry to fill teeth.
Is it safe?
Absolutely! Mercury is toxic. It is also a component of amalgam restorations. However, once the filling material is set, mercury does not escape and cause harm. Water is a fine analogy. Water is made up of Hydrogen (a highly combustible gas) and Oxygen (an element required for combustion). We drink water daily without fear of exploding!
For more information, see the article below.
Advantages of Amalgam:
- It is inexpensive. (Relatively!)
- It is durable.
- It is stronger.
- It is forgiving. (Can be placed in difficult environments.)
- It has stood the test of time.
Disadvantage:
- It is UGLY!
Amalgam Safety
National Council Against Health Fraud
119 Foster Street, Bldg. R, 2nd Floor, Peabody, MA 01960
(978) 532-9383 ||| www.ncahf.org ||| ncahf.office@verizon.net
Position Paper on
Amalgam Fillings
Background History
Dental amalgam has been widely used for over 150 years. It is made by mixing approximately equal parts of elemental liquid mercury (43 to 54 percent) and an alloy powder (57 to 46 percent) composed of silver, tin, copper, and sometimes smaller amounts of zinc, palladium, or indium [1]. Although some forms of mercury are hazardous, the mercury in amalgam is chemically bound to the other metals to make it stable and safe for use in dental applications.
The difference between bound and unbound chemicals can be illustrated by a simple comparison. Elemental hydrogen is an explosive gas. Elemental oxygen is a gas that supports combustion. When combined, however, they form water, which has neither of these effects. Saying that amalgam will poison you is like drinking water will make you explode and burst into flames.
Amalgam is the most thoroughly studied and tested filling material now used. Compared to other restorative materials, it is durable, easy to use, and inexpensive. The American Dental Association, Consumers Union, the U.S. Food and Drug Administration, the U.S. Public Health Service, the World Health Organization, and many other prominent organizations have concluded that amalgam is safe and effective for restoring teeth [2-6]. It is safe to assume that if a better material is developed, the dental profession will adopt and use it.
Amalgam Safety
The amount of mercury released from installed amalgam and absorbed by the body is minuscule. Mercury is found in the earth's crust and is ubiquitous in the environment. Thus, even without amalgam fillings, everyone has small but measurable blood and urine levels. Amalgam fillings may raise these levels slightly, but this has no practical or clinical significance.
The legal limit of safe mercury exposure for industrial workers is 50 micrograms per cubic meter of air for 8 hours per day and 50 weeks per year. Regular exposure at this level will produce urine mercury levels of about 135 micrograms per liter. These levels are much higher than those of the general public but produce no symptoms and are considered safe.
Most people with fillings have less than 5 micrograms per liter of urine. Nearly all practicing dentists have levels below 10 micrograms per liter, even though they are exposed to mercury vapor when placing or removing amalgam fillings and typically have amalgams in their own teeth. Thus, even with that exposure, the maximum levels found in dentists are only slightly higher than those of their patients and are far below the levels known to affect health, even in a minor way [7-12].
No illness has ever been associated with amalgam use in patients, except for rare allergies. Moreover, there is insufficient evidence to assure that components of other restorative materials have fewer potential health effects than dental amalgam, including allergic reactions.
Improper Claims
Despite the above facts, some dentists and other health professionals advise people to avoid amalgam and to have their amalgam fillings replaced with other materials. Dentists who oppose the use of amalgam may refer to their approach as holistic dentistry, biological dentistry, or mercury-free dentistry.
Offbeat practitioners often diagnose "amalgam toxicity" or "amalgam illness" in patients who suffer from multiple common symptoms. One study found that people with symptoms related to amalgam fillings did not have mercury blood and urine mercury levels that were significant or higher than those of a control group [12]. Several studies have found that many symptoms attributed to amalgam restorations are psychosomatic and have been exacerbated by information from the media or a dentist [13-17]. False diagnoses of "mercury toxicity" are also made by many of the physicians who offer chelation therapy, a series of intravenous infusions that costs thousands of dollars.
The leading anti-amalgamist has been Hal Huggins, D.D.S., of Colorado Springs, Colorado. Huggins claims that "sensitive" individuals can develop emotional problems (depression, anxiety, irritability), neurological disorders (facial twitches, muscle spasms, epilepsy, multiple sclerosis), cardiovascular problems (unexplained rapid heart rate, unidentified chest pains), collagen diseases (arthritis, scleroderma, lupus erythematosus), allergies, digestive problems (ulcers, regional ileitis), and immunologic disorders (which he claims include leukemia, Hodgkin's disease, and mononucleosis). He recommends replacing amalgam with other materials and taking vitamins and other supplements to prevent trouble after amalgam removal [18]. There is no scientific evidence that amalgam fillings cause or contribute to developing these diseases.
Huggins's dental license was revoked in 1996. During the revocation proceedings, the administrative law judge concluded:
- Huggins had diagnosed "mercury toxicity" in all patients who consulted him in his office, even some without mercury fillings.
- He had also recommended extraction of all teeth with root canal therapy.
- Huggins's treatments were "a sham, illusory and without scientific basis." [19]
- A practitioner who does not wish to use amalgam can still practice ethically by giving appropriate advice and referring patients elsewhere when amalgam is the best choice. But advertising practice as "mercury-free" is unethical because it falsely implies that amalgam fillings are dangerous and that "mercury-free" methods are superior.
Dubious Tests
The advice from anti-amalgam practitioners is typically accompanied by one or more tests that are either misinterpreted or downright bogus.
Breath Testing. Breath testing involves probing the mouth with a vacuum device after the patient chews gum vigorously for several minutes. The procedure causes tiny amounts of mercury to be released from amalgam fillings and deposited on a gold foil within the device. Because people only chew during a small part of the day, the resultant readings are much higher than the average amounts released per 24 hours. In addition, the amounts deposited the foil are artificially high because most mercury vapor is exhaled rather than absorbed by the body and the device remeasures the same air several times, which inflates the reading. The readouts of the device are also raised by the presence of traces of foods, bacterial gases, and other substances commonly found within the mouth.
Urine Testing. Because mercury is ubiquitous, the body reaches a steady-state in which tiny amounts are absorbed and excreted. Thus, mercury is commonly found in people's urine. Mercury can also be found in the blood because this is the major medium for transporting materials around the body. Large-scale studies have shown that the general population has urine-mercury levels below ten micrograms/liter. Industrial workers, and dentists, who have regular exposure to mercury vapor also have low values. Urine testing, a fairly reliable indicator of chronic exposure, is best performed on a 24-hour urine specimen. Urine mercury levels can be temporarily raised by administering a chelating agent such as DMSA or DMPS, which collects the small amounts of mercury from the body, concentrates them, and then forces them to be excreted. In other words, mercury that recirculates typically within the body is now bound and excreted. The urine level under such circumstances is artificially raised above the steady-state level. The use of a chelating agent before testing should be considered fraudulent.
Blood Testing. Mercury is excreted by the kidneys, which filter the blood. The mercury levels in the blood are lower than those of urine and, therefore, more difficult to detect. Even at high levels of mercury exposure, industrial workers show blood concentrations in the parts-per-billion range, typically less than five parts per billion. In this range, the amounts are too small to identify the type of mercury or its source. Urine mercury testing gives a more meaningful picture of exposure and is also more accurate because the mercury is more concentrated.
Skin Testing. Some anti-amalgamists administer a "patch test" with a dilute solution of corrosive mercury salts that cause the skin to redden and swell [20]. The reaction is misinterpreted as a sign of mercury allergy or toxicity.
Stool Testing. Fecal mercury levels are not an accurate indicator of mercury exposure. The amount found in stool reflects the amount eaten and not absorbed, plus anything excreted in the stool. At best, a stool test might indicate that mercury entered the gastrointestinal tract. Still, it could not provide an accurate measurement of either exposure or what was absorbed into the body.
Hair Analysis. Hair analysis is performed by sending a hair sample to a commercial hair analysis laboratory, which issues a computerized report indicating the number of micrograms found and whether that amount should be considered harmful. This procedure is not valid. Hair contains trace amounts of mercury from food, water, and air, regardless of whether the person has amalgam fillings. Because hair can absorb mercury from external sources, the amount of mercury it contains does not necessarily reflect the amount within the body. In addition, hair mercury testing cannot be standardized because hair thickness, density, shape, surface area, and growth rate vary from person to person. The laboratory used most for hair analysis is Doctor's Data of Chicago, which reports "toxic mineral" levels as "high" when the amounts are near the top of their "reference range." [21] This means that the specimen contained more than most other hair specimens handled by the lab. It does not mean that the level is abnormal or that the level within the patient's body is dangerous. Thus even if hair analysis were valid, the reporting process is not.
Electrodermal Testing. Some practitioners use quack diagnostic devices that are said to detect "electromagnetic imbalances." One wire from the device goes to a brass cylinder that the patient holds in one hand. A second wire is connected to a probe, which the operator touches various points inside the mouth. This completes a low-voltage circuit, and the device registers the flow of current, which the operator misinterprets as abnormal.
Physical Harm
Improper removal of amalgam fillings is usually followed by replacement with a more costly material. But removing good fillings is not merely a waste of money. In some cases, it results in significant damage or loss of the tooth. To remove an intact filling, it is necessary to drill into the tooth around the outer edges of the amalgam. If the filling is large or deep, the tooth can be significantly weakened, and the heat from the drilling process can injure the relatively delicate tissues of the pulp beneath the filling. To this risks must be added the general risks of anesthesia and other types of mechanical injury that are uncommon but are inexcusable when a procedure is unnecessary.
In 1985, a $100,000 settlement was awarded to a 55-year-old California woman whose dentist removed her amalgam fillings. Based on testing with a phony electrodiagnostic device, the dentist had claimed that six of her fillings were a "liability" to her large intestine [22]. In removing the fillings, the dentist caused severe nerve damage necessitating root canal therapy for two teeth and extraction of two others.
Regulatory Action
The American Dental Association Council on Ethics, Bylaws, and Judicial Affairs have concluded that "removal of amalgam restorations from the non-allergic patient solely for the alleged purpose of removing toxic substances from the body, when such treatment is performed at the recommendation or suggestion of the dentist, is improper and unethical." [23] The policy, initiated in 1986, was triggered in part by the case of an Iowa dentist who had extracted all 28 teeth of a patient with multiple sclerosis. The dentist received a 9-month license suspension followed by 51 months of probation.
Dentists who attempt to "diagnose" or "treat" "heavy metal toxicity" or who test patients for heavy metals by any means are not practicing dentistry. These activities fall outside the scope of dental licensure. Any dentist who believes a patient requires diagnosis or treatment for any medical condition outside of the scope of dentistry is obliged to make a referral to a physician or other health professional as appropriate. Failure to make such a referral should be considered negligence.
Selection of material should be based only on its known clinical properties and performance for the particular placement situation, coupled with the needs of a patient. A dentist who excludes any material from possible selection for a given restoration on the sole basis of personal opinion or unsupported conjecture cannot be providing optimal services for all of their patients. Such a dentist may be denying a patient the benefits of a material that is most suitable for that patient's needs. Such denial should be considered unprofessional conduct.
No dentist is required to use amalgam. However, dentists who make false claims about amalgam safety create unnecessary patient anxiety and undermine confidence in the profession. Such behavior should be considered unprofessional conduct. Consumers Union (C.U.) has concluded:
Dentists who purport to treat health problems by ripping out fillings put their economic interests ahead of their patient's welfare. The false diagnosis of mercury-amalgam toxicity has such harmful potential. It shows such poor judgment of the practitioner that C.U. believes dentists who engage in this practice should have their license revoked [24].
Legal and Political Action
Class-action suits have been filed in Maryland and California, claiming that patients have been harmed by amalgam fillings and that the American Dental Association (A.D.A.) and state dental associations have engaged in unfair and deceptive trade practices as well as fraud and conspiracy to defraud by not informing patients that amalgam fillings contain mercury. The A.D.A. has countered that the suits are part of a "coordinated attempt by some to have judges decide matters of scientific debate, and stifles discussion within the scientific community, most of whose members simply do not agree with their views." [25] In a news report, an A.D.A. official referred to a California suit as "an egregious abuse of the legal system." [26] NCAHF concurs with this assessment.
U.S. Representative Diane Watson (D-CA) has introduced a bill to prohibit interstate commerce of mercury intended for use in dental fillings by 2007. She does not appear to understand that the properties of chemical combinations can differ significantly from those of the individual ingredients that form them. Calling Watson "scientifically unsophisticated," Time magazine science writer Leon Jaroff has urged Watson to get over her "amalgam hang-up" and "learn not to be taken in by quacks." [27] NCAHF hopes that she will do so.
Recommendations
To Consumers
- There is no logical reason to worry about the safety of amalgam fillings.
- Anyone told that a urine mercury level produced after taking DMPS represents a toxic state is being misled.
- Avoid health professionals who advise you that amalgam fillings cause disease or should be removed as a "preventive measure."
- Report any such advice to the practitioner's state licensing board.
To Dental Organizations
- Issue clear and forceful guidelines indicating that unnecessary amalgam removal is unethical and unprofessional and that the diagnosis of mercury toxicity is outside the proper scope of dentistry.
- Issue a position statement about dubious mercury testing
To Dental Licensing Boards
- Practice standards should be based solely on scientifically gathered objective evidence.
- Classify as unprofessional conduct any advice that amalgam fillings are dangerous and therefore should be avoided or removed.
- Ban the use of hair analysis and chelating agents by dentists.
- Ban any advertising of "mercury-free dentistry" which falsely implies that amalgam fillings are dangerous and should therefore be avoided or removed.
To Legislators
- Do not be misled by false claims that amalgam is dangerous.
- Do not support special laws that would restrict or discourage amalgam use.
References
- Dental amalgam use and benefits. U.S. Centers for Disease Control Resource Library Fact Sheet, December 2001.
- A.D.A. Council on Scientific Affairs. Dental amalgam: Update on safety concerns. JADA 1998;129:494-501.
- The mercury in your mouth. Consumer Reports 1991;56:316-319.
- Benson JS and others. Dental Amalgam: A Scientific Review and Recommended Public Health Strategy for Research, Education and Regulation. Washington, DC: U.S. Public Health Service, 1993.
- Consumer Update: Dental amalgams. F.D.A. Center for Devices and Radiological Health, Feb 11, 2002.
- World Health Organization. Consensus Statement on Dental Amalgam. Mjor IA, Pakhomov GN. Dental Amalgam and Alternative Direct Restorative Materials. Geneva: World Health Organization, 1999.
- Mackert JR. Dental amalgam and mercury. JADA 1991;122:54-61.
- Olsson S, Bergman M. Daily dose calculations from measurements of intra-oral mercury vapor. J Dent Res 1992;71:414-423.
- Mackert JR. Factors affecting estimation of dental amalgam exposure from measurements of mercury vapor in levels in intraoral and expired air. J Dent Res 1987;66:1175-1180.
- Mackert JR Jr, Berglund A. Mercury exposure from dental amalgam fillings: absorbed dose and the potential for adverse health effects. Crit Rev Oral Biol Med 1997;8:410-436.
- Berglund A. Molin M. Mercury vapor release from dental amalgam in patients with symptoms allegedly caused by amalgam fillings. Eur J Oral Sci 1996;104:56-63.
- Dodes J. The amalgam controversy: An evidence-based analysis. JADA 2002;132:348-356.
- Herrstrom P, Hogstedt B. Clinical study of oral galvanism: No evidence of toxic mercury exposure but anxiety disorder an important background factor. Scand J Dent Res 1993;101:232-237.
- Lindberg NE, Lindberg E, Larsson G. Psychological factors in the etiology of amalgam illness.. Acta Odontol Scand 1994;52:219-228.
- A multidisciplinary clinical study of patients suffering from illness associated with mercury release from dental restorations: Psychiatric aspects. Acta Psychiatr Scandinavia 1997;96:475-482.
- Malt UF, Nerdrum P, Oppedal B, et al. Physical and mental problems attributed to dental amalgam fillings: a descriptive study of 99 self-referred patients compared to 272 controls. Psychosom Med 1997;59:32-41.
- Bailer J, Rist F, Rudolf A, at el. Adverse health effects related to mercury exposure from dental amalgam fillings: toxicological or psychological causes? Psychol Med 2001;31:255-263.
- Huggins HE, Huggins SA. It's All in Your Head. Self-published, Colorado Springs, Colorado,1985.
- Connick N. Before the State Board of Dental Examiners, State Board of Colorado. Case No. 95-04. In the matter of the disciplinary proceedings regarding the license to practice dentistry in the State of Colorado of Hal A. Huggins, D.D.S., License No. 3057. Feb 29, 1996.
- Fisher AA. The misuse of the patch test to determine "hypersensitivity" to mercury amalgam dental fillings. Cutis 1985;35:109, 112, 117.
- Druyan ME and others. Determination of reference ranges for elements in human scalp hair. Trace Elem Res 1998;62:183-197.
- Sherry v Doe. California Sonoma County Superior Court, No. 134740, March 1, 1985.
- Dental amalgam and other restorative materials. Advisory opinion 5.A.1, American Dental Association Principles of Ethics and Code of Professional Conduct, revised April 2002.
- Barrett S and the editors of Consumer Reports. Health Schemes, Scams, and Frauds. New York: Consumer Reports Books, 1990.
- Berry J. A.D.A. pledges vigorous defense' against Maryland amalgam suit. A.D.A. News March 4, 2002.
- Another amalgam suit filed in California. A.D.A. news release, March 21, 2002.
- Jaroff, L.
There's nothing dangerous about 'silver' fillings: But some in Congress continue to insist there is.
http://www.time.com. May 8, 2002.
Root Canal Therapy
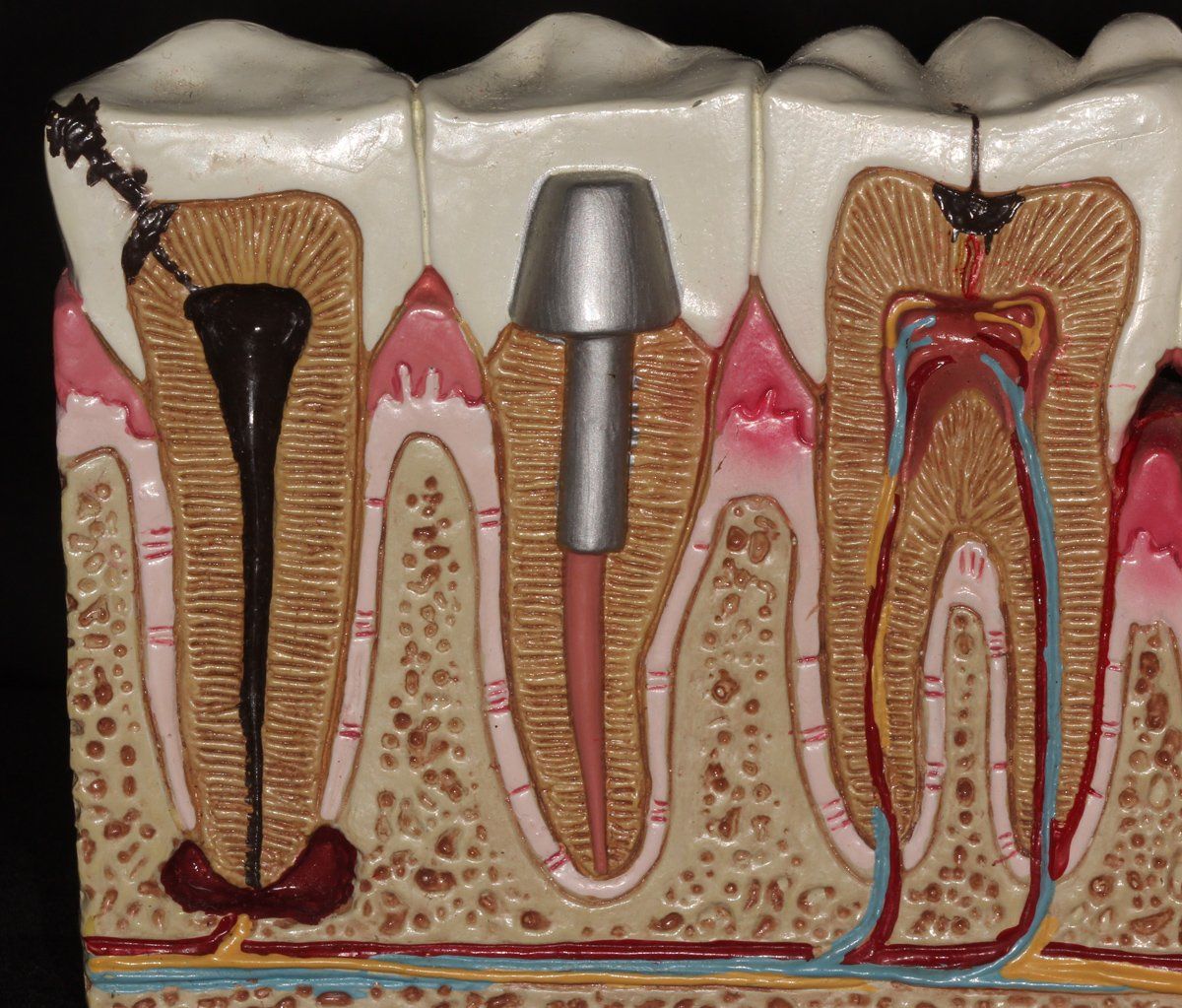
What is it? Root canal therapy is a treatment used to repair and save a tooth that has been infected due to a deep cavity or crack. The treatment involves removing the nerve and pulpal tissues of the tooth, cleaning the infected area, and placing a rubber-like filling material in the canal once occupied by the nerve. If the treatment is not performed, pus builds up at the root tip, and the pulp infection can spread to the surrounding bone. In the picture above:
- The tooth on the far right has normal pulpal tissues but a cavity starting on the biting surface.
- The tooth on the far left has an infected nerve due to a cavity.
- The tooth in the middle has a completed root canal and filling.
What are the signs that a root canal is needed?
- Severe pain while chewing.
- Tooth pain that wakes you up at night.
- Lingering hot/cold sensitivity.
- Discoloration or darkening of the tooth.
- Swollen gums in the area of the infected tooth.
- Sensitivity to percussion or tapping pressure.
What does the treatment involve?
First, an opening is made into the pulp chamber through the tooth's crown. Once the pulp is removed, the root canal is thoroughly cleaned. Most teeth with a root canal will benefit from a buildup restoration or a post and core followed by a crown. Teeth that have had root canals are easier to fracture than those that have not had root canals.
Do root canals hurt?
THEY CAN! If a tooth is ignored until the pain is “out of control” and the infection is severe, the infection can block or limit the effectiveness of dental anesthesia. It is best to seek professional attention immediately when a toothache starts or when one of the signs/symptoms listed above are present.
MOST OF THE TIME, ROOT CANALS CAN BE DONE PAINLESSLY! However, the tooth and its symptoms must be managed appropriately to facilitate painless treatment.
Tooth Extractions
An extraction is a procedure to remove a tooth. Extraction is most commonly required if one of your teeth is damaged beyond practical repair. The most common reasons for tooth extractions include:
- Severe decay or infection.
- Advanced gum disease.
- Space discrepancy. (Especially Wisdom teeth)
Dental Exams and X-Rays
Beautiful smiles don’t just “happen” by chance. If you are fortunate enough to have a beautiful God-given smile, much work is involved in maintaining it for a lifetime. Routine dental exams are essential to maintaining healthy teeth and gums. Additionally, they can help avoid the financial costs associated with large treatment plans later on. Dr. Houston recommends twice yearly checkups for people of all ages. At this frequency, most problems can be caught early.
How it's done:
There are many essential components to an excellent overall exam, including:
- Medical history review: Dr. Houston and staff will assess how any medical conditions or illnesses may affect your dental health.
- Examination of tooth decay: Your mouth will be checked for cracked or decayed teeth. Often this is done with a Diagnodent laser or a Spectra camera. Each of these devices uses light to find decay and other problems. X-rays are an essential part of this exam.
- Oral cancer screening: The face, neck, lips, tongue, throat, tissues, and gums will be checked for any signs of oral cancer.
- Gum disease evaluation: Your gums and bone around the teeth will be checked for any evidence of periodontal disease.
- Examination of existing restorations: Current fillings, crowns, and other restorations are made sure to be in good order.
- T.M.J. evaluation: Your jaw joints and associated muscular structures will be evaluated.
- Radiographic evaluation: Dr. Houston will recommend diagnostic x-rays to reveal any other hidden problems, especially in the areas below the gums. Bitewing x-rays are typically taken every 12 months, and a panographic x-ray, which revolves around the head, is taken every three years.
We’d love to hear from you! Call our friendly team at 864-439-3322.






